I work in a nanofabrication facility using high-vacuum tools and sophisticated radio frequency (RF) systems to generate plasmas (that will be a topic for another day!). These machines are designed to strip away atoms from surfaces with extraordinary precision, etching nanoscale features into silicon wafers. We used RF power to ionize gases like argon or oxygen, creating highly reactive plasmas. These plasmas are not only beautiful to watch through the viewports — glowing blue or purple depending on the gas — but also undeniably powerful. I have a healthy respect for what electromagnetic radiation can do under the right circumstances. As for David, his PhD was on ultraviolet radiation, a form of higher energy light that can cause skin cancer, before he went into radiotherapy - the use of EXTREMELY high energy light to break DNA apart - in this case, the DNA of cancer cells. Between the pair of us, we’d be the first to tell you that there are some forms of electromagnetic radiation you’d really rather avoid.


Being exposed directly to a plasma can definitely be dangerous (some plasmas are extremely hot, some may contain chemically reactive radicals like atomic oxygen or fluorine, which can aggressively react with organic tissue, etc.), but here’s the catch: the radio waves that generate them aren’t dangerous themselves. The RF fields we use are just a tool to energize gas molecules inside a tightly controlled vacuum chamber. Outside of the chamber? Totally harmless. You could stand right next to the tool and feel nothing. This distinction — between energy applied in a specific context versus ambient exposure — is key to understanding the entire debate around cell phones, Wi-Fi, and cancer risk.
Understanding the Relationship between Wave Properties and Energy
Let’s start with the basics: radio waves are part of the electromagnetic (EM) spectrum, which includes all types of electromagnetic radiation, from very low-frequency radio waves to extremely high-frequency gamma rays. Electromagnetic radiation is a form of energy that travels through space as waves made up of oscillating electric and magnetic fields. These waves move at the speed of light and do not require a medium to travel — they can move through air, solid materials, or even the vacuum of space.
The critical thing to understand is that the energy of electromagnetic radiation increases with frequency and decreases with wavelength. This relationship is governed by the equation:
E = hf, where:
E is the energy of a photon,
h is Planck’s constant (6.626×10−34 joule·seconds), and
f is the frequency of the wave.
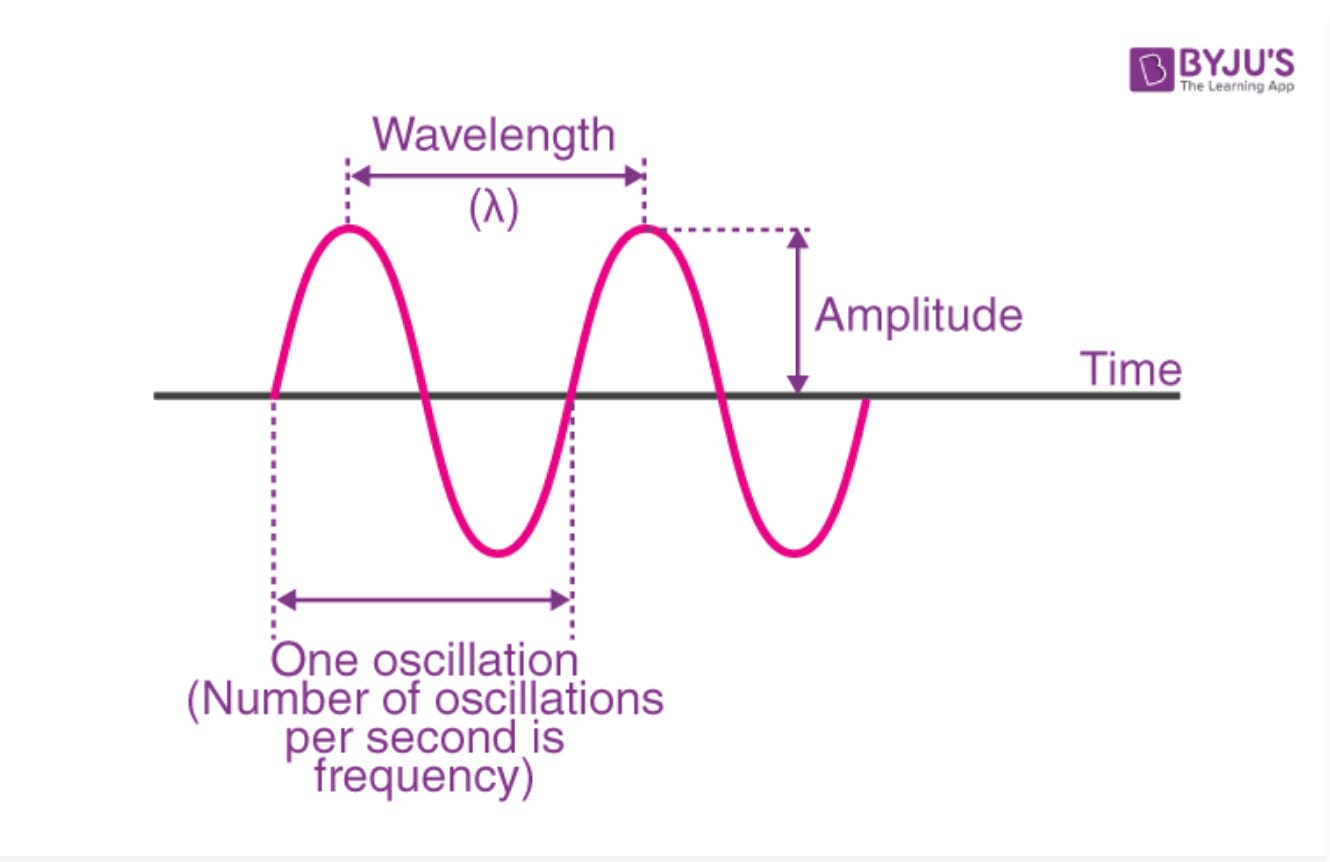
To better understand this, let’s look at the fundamental properties of a wave:
Wavelength (λ): This is the distance between two consecutive peaks (or troughs) of a wave. In EM radiation, longer wavelengths correspond to lower frequencies.
Frequency (f): Measured in hertz (Hz), frequency is the number of wave cycles that pass a point in one second. Higher frequencies mean more energy.
Amplitude: This is the height of the wave and relates to the intensity or strength of the wave, but not its energy per photon.
Speed (c): All electromagnetic waves travel at the speed of light in a vacuum (approximately 3.0 x 10^8 meters per second). This means that wavelength and frequency are inversely related by the equation:
c = λf, where:
c is the speed of light,
λ is wavelength,
f is frequency.
So, when you know the frequency of a wave, you can calculate its wavelength, and vice versa. And once you know the frequency, you can also determine its photon energy using Planck’s equation.
Radio waves are at the far end of the EM spectrum, with the lowest frequencies (from kilohertz to gigahertz), the longest wavelengths (from millimeters to thousands of meters), and the lowest photon energies. For example, a 2.4 GHz Wi-Fi signal corresponds to photons with energies around 1 x 10^-5 electron volts (eV) or 9.93μeV to be exact — far too low to break any chemical bonds.
Compare that to X-rays (100-1000 eV), or gamma rays (over 1 million eV), all of which are forms of ionizing radiation. Ionizing radiation, which has much higher frequencies, has enough energy to strip electrons from atoms. As ionizing photons pass through tissue, some are absorbed by molecules, releasing their energy. This creates fast-moving charged particles. These particles can damage DNA directly or react with water to form harmful radicals that, in turn, damage DNA indirectly. This is the kind of radiation used in medical imaging or emitted during nuclear reactions — and it is proven to increase cancer risk with sufficient exposure.

These effects are dose-dependent and well-documented across epidemiology and animal studies. A few exposures here and there for X-rays will amount to a negligible risk (in fact one X-ray is comparable to about a daily background radiation dose). By contrast, constant exposure to radon gas, a natural emitter of ionizing alpha particles, can certainly increase your risk of lung cancer (coming close second in the U.S. after smoking). According to recent estimates, the average person in the U.S. receives an effective dose of about 3 mSv per year from natural radiation, which includes cosmic radiation from outer space, terrestrial sources, and internal radionuclides.

Non-ionizing radiation — which includes everything from visible light to microwaves to radio waves — simply does not carry enough energy per photon to cause the kind of damage ionizing radiation can.It can certainly cause heating effects, which is the principle behind how a microwave oven works (and relevant later on). But even then, the power levels involved in many consumer electronics are thousands of times lower than what would be required to cause excess heating of tissues.
Understanding this energy spectrum and the fundamental difference between ionizing and non-ionizing radiation is crucial. The public conversation about cell phones and Wi-Fi often skips this, leading to misplaced fears. It’s not just about whether radiation is present — it’s about what kind of radiation it is, and how much energy it carries.
What about our mobile devices?
Most mobile devices operate within the RF-EMF frequency range of 700 MHz to 2.6 GHz, depending on the network generation and region. Here's a breakdown:
2G / 3G: Typically use 850 MHz, 900 MHz, 1800 MHz, and 1900 MHz bands.
4G (LTE): Operates in a range between 700 MHz and 2.6 GHz, depending on carrier and country.
5G:
Sub-6 GHz (FR1): Includes frequencies below 6 GHz, such as 3.5 GHz – widely used globally.
mmWave (FR2): Uses higher frequencies, typically 24 GHz to 40 GHz – mostly in urban or dense environments.
Visible light photons typically have energies ranging from about 1.65 eV to 3.1 eV, depending on the wavelength. In Europe, the 5G spectrum spans from 3.6 GHz to 26 GHz. At these frequencies, even the most energetic 5G RF photon has over 15,000 times less energy than the weakest photon of visible light.
In the sections that follow, we’ll dive deeper into the science, epidemiology, and expert consensus to understand why — despite decades of study — there is still no compelling evidence that the kind of radiofrequency radiation emitted by your phone or Wi-Fi router causes cancer.
Going back to rodent data
The more hotly debated evidence around cell phones comes from a few animal studies. In 2018, the U.S. National Toxicology Program (NTP) reported results from a multi-year experiment that blasted rats and mice with cell phone-frequency radiation (2G and 3G signals) at high levels for their entire lifetimes. The exposures (up to 9 watts per kilogram) were much higher than what people get from phones – the rodents endured whole-body RF exposure for about 5 or 7 days per week for 18 hours per day in cycles of 10 minutes on, 10 minutes off (so about 9 hours total). Most cell phones are regulated to stay below 1.6 W/kg (U.S.) or 2 W/kg (Europe) - this is the Specific Absorption Rate (SAR).
The findings: male rats showed a small increase in some rare tumors (malignant Schwann cell tumors in the heart). Female rats did not show this, nor did any of the mice, and no clear increase in brain tumors was seen. Curiously, the high-exposure male rats also lived longer than the unexposed control rats. Around the same time, an Italian study found a higher incidence of the same rare tumor in male rats exposed to RF resembling cell tower emissions. These results grabbed headlines – “Cell Phone Radiation Causes Cancer in Rats!” – and indeed they suggested that under certain conditions (very high, prolonged RF exposure), biological effects seemed to occur in rodents. The only problem was that when other researchers investigated this, they found nothing beyond statistical fluke, a classic example of a false positive born of some questionable statistical choices by the experimenters.
In any case, it’s a big leap to apply this to humans using phones. First, the exposure levels in those studies were far above what typical phone users experience (phones operate under strict limits to avoid overheating tissue). Second, the pattern of tumors was odd and limited to one sex and one species, which the authors could not explain. Third, the types of tumors observed (heart schwannomas) are extremely uncommon in people. An independent expert review of these studies noted some major weaknesses in how they were conducted and analyzed, concluding that those limitations “prevent drawing conclusions about [RF’s] ability to cause cancer.” In addition, a very strong confounder is that exposed groups lived longer - cancer is related to age, so it is unclear if the higher risk was driven by age or RF exposure.
Like with ingredients, we have guardrails to limit exposure
Mobile phones are tested under the worst-case scenario — meaning they're measured at their maximum possible power output. For example, while a phone might be capable of sending out 2 watts of peak power, the average power actually used is usually much lower — around 250 milliwatts for a GSM (2G) phone at 900 MHz.
In real-world use, the amount of radiation your body absorbs (measured as SAR) typically ranges from 0.2 to 1.5 W/kg, depending on the phone model. But here’s the key: phones rarely operate at full power. Because of features like power control and discontinuous transmission (your phone uses less power when you're listening than when you're speaking), the actual exposure is far lower.
In fact, your phone can automatically reduce its power output by up to 1,000 times (for GSM) or even by a factor of 100 million (for UMTS/3G networks) when full strength isn’t needed. So, although phones are tested at their highest output, real-life exposure is usually much, much lower.
In plain English, the animal evidence is suggestive but not conclusive, and may not translate to normal human use. At most, these studies justify continued research to understand any possible effects, but they do not demonstrate that cell phones will cause cancer in real-world conditions. This is analogous to when we look at the thresholds for substances like food additives and pesticides by identifying the No Observed Effect Level (NOEL) or No Observed Adverse Effect Level (NOAEL) from animal studies, which is the highest dose with no harmful effects.
Has Brain Cancer Become More Common in Humans Since Cell Phones Became Widespread?
Surprisingly, to some, the answer is, to date, no.
Studies on the health effects of radiofrequency (RF) radiation have been grouped into two main categories based on frequency ranges:
Lower Frequencies (FR1: 450–6,000 MHz):
This range includes the frequencies used by current 2G, 3G, and 4G networks. Since these technologies have been in use for many years, the available research on them provides the most reliable and extensive evidence.Higher Frequencies (FR2: 24–100 GHz):
These are millimeter waves (MMW) used in new 5G networks, and they have different physical properties — such as shallower skin penetration and higher energy per photon. Since these frequencies are new to mobile communications, research on them is still emerging and was assessed using a scoping review approach, which is broader and more exploratory.
In short, we have solid data on the health effects of older mobile networks (2G–4G), while studies on the new high-frequency 5G bands are still in early stages.
Here is a summary of some the data (this is a very good resource):
Despite the explosion in global cell phone use over the past few decades, the incidence of brain and central nervous system cancers has remained stable. Large-scale population studies in multiple countries — including the United States, Nordic countries, and Australia — have not observed any significant rise in adult glioma cases over time. Similarly, rates of pediatric brain tumors in the U.S. remained steady from 1993 to 2013. Rates for specific nonmalignant tumors, like acoustic neuroma and meningioma, have also not increased since 2009, despite more widespread cell phone adoption. During these time periods adoption of cell phones rose across the globe.
It’s important to note that these population-level studies track overall trends, so they’re better at detecting broad shifts rather than very small increases in rare subgroups or heavy users. To examine more subtle effects or risks in specific populations, researchers turn to observational studies like case–control and cohort studies, which are designed to measure individual exposure and link it to health outcomes.
Case–control studies, compare cell phone use between individuals with tumors and those without, and cohort studies follow groups of people over time to observe if those who use cell phones are more likely to develop tumors. The cancers examined include both malignant tumors like gliomas (a type of brain cancer) and nonmalignant tumors such as acoustic neuromas, meningiomas, parotid gland tumors, skin cancers, and thyroid tumors.
Major Findings from Key Studies
1. Interphone Case-control Study:
The largest international study of its kind, Interphone collected data from participants in 13 countries. Overall, it found no clear increase in brain or nervous system cancers from cell phone use. A slight rise in glioma risk was seen in the highest-use group, but this was considered inconclusive. Some analyses hinted at higher tumor rates in the areas of the brain exposed to the phone, but results were inconsistent.
2. Danish Cohort Study:
Using phone subscriber data from over 358,000 individuals, this study found no link between cell phone use and risks for glioma, meningioma, or acoustic neuroma — even in long-term users.
3. COSMOS Study (Europe):
Following over 260,000 people, this ongoing study found no increased cancer risk — even among long-term or heavy users of mobile phones.
Findings from Other Studies
Several smaller or national studies also generally support these findings:
Two U.S. NCI-sponsored studies found no increased risk of brain tumors in adults.
A Connecticut study found no link between phone use and thyroid cancer.
Furthermore, numerous other studies, as selected from the Europe Parliamentary Research Service found weak or absent correlations.
An exception to this is a combined Swedish study that found a statistically significant increase in brain cancer risk with greater cell phone use among individuals who started using phones before age 20. However, this finding was strongly challenged by another analysis, which argued that the reported risk increase was inconsistent with actual glioma rates observed in the Nordic countries. Additional analysis of incidence data from 1974 to 2008 in these countries also showed no rise in age-adjusted brain tumor rates.
Epidemiological studies, albeit limited in number, considering exposures from 24GHz to 100 GHz (higher frequencies) did not show strong associations between these radio frequencies and selected cancers (glioma, meningioma, uveal melanoma and testicular cancer) either.
The International Agency for Research on Cancer (IARC) reviewed studies on whether work-related exposure to radiofrequency (RF) radiation — including the higher frequencies used in 5G— is linked to cancer. Their conclusion?
For brain tumors, there was no clear evidence of a connection. The studies had flaws, like inaccurate exposure estimates and other factors that may have skewed results.
For leukemia and lymphoma, there were some weak signs of a possible link, but the studies weren’t reliable enough to draw firm conclusions because of limited data and potential confounding factors.
Some studies also hinted at a possible connection between RF exposure and other cancers (like eye cancer, testicular cancer, breast, lung, or skin cancer), but the findings were inconsistent and the study quality was often poor.
As of now, only three studies have looked at health effects specifically from 5G’s highest frequencies— and none were strong enough to establish a clear link.
The Canary in the Goldmine: Occupational Exposure and Higher RF
When evaluating the potential link between RF radiation and cancer, several key factors diminish the likelihood of a causal relationship.
First, the lack of a dose-response relationship is a significant weakness in the argument for causality. If RF radiation were a carcinogen, we would expect to see higher rates of cancer with increasing frequency or intensity of exposure. However, this is not consistently observed. In fact, three studies on occupational exposures involving radar operators or individuals working near radar stations—who are exposed to higher frequency RF-EMFs—did not show any clear association between these exposures and increased cancer risk. This undermines the expectation that higher frequencies (and therefore potentially higher energy exposures) would lead to greater cancer incidence.
Second, epidemiological studies on occupational exposure to RF-EMF, including workers exposed to a range of frequencies in industrial, military, or communication settings, have explored possible links to brain tumors, leukemia, lymphoma, and cancers of the breast, lung, skin, testis, and others. However, these studies have generally produced inconsistent results and suffered from methodological limitations, such as poor exposure assessment, recall bias, and uncontrolled confounding factors.
Importantly, studies examining environmental RF-EMF exposure in the general population also fail to provide sufficient evidence for a clear conclusion. This suggests that if there is any risk at all, it is likely to be very small or nonexistent, particularly given widespread environmental exposure with no clear rise in related cancers at the population level.
In sum, the absence of a dose-response trend, the weak or inconclusive data in high-exposure occupational groups, and the general lack of consistent findings across studies strongly suggest that RF radiation is unlikely to be a significant cause of cancer.
What about other health effects?
The potential impact of radiofrequency electromagnetic fields (RF-EMF), such as those emitted by mobile phones and other wireless devices, on fertility has been the subject of various studies as well. This data spans male and female fertility, and pregnancy or neonatal outcomes. There are In-vitro, animal, and human (epidemiological) studies to consider.
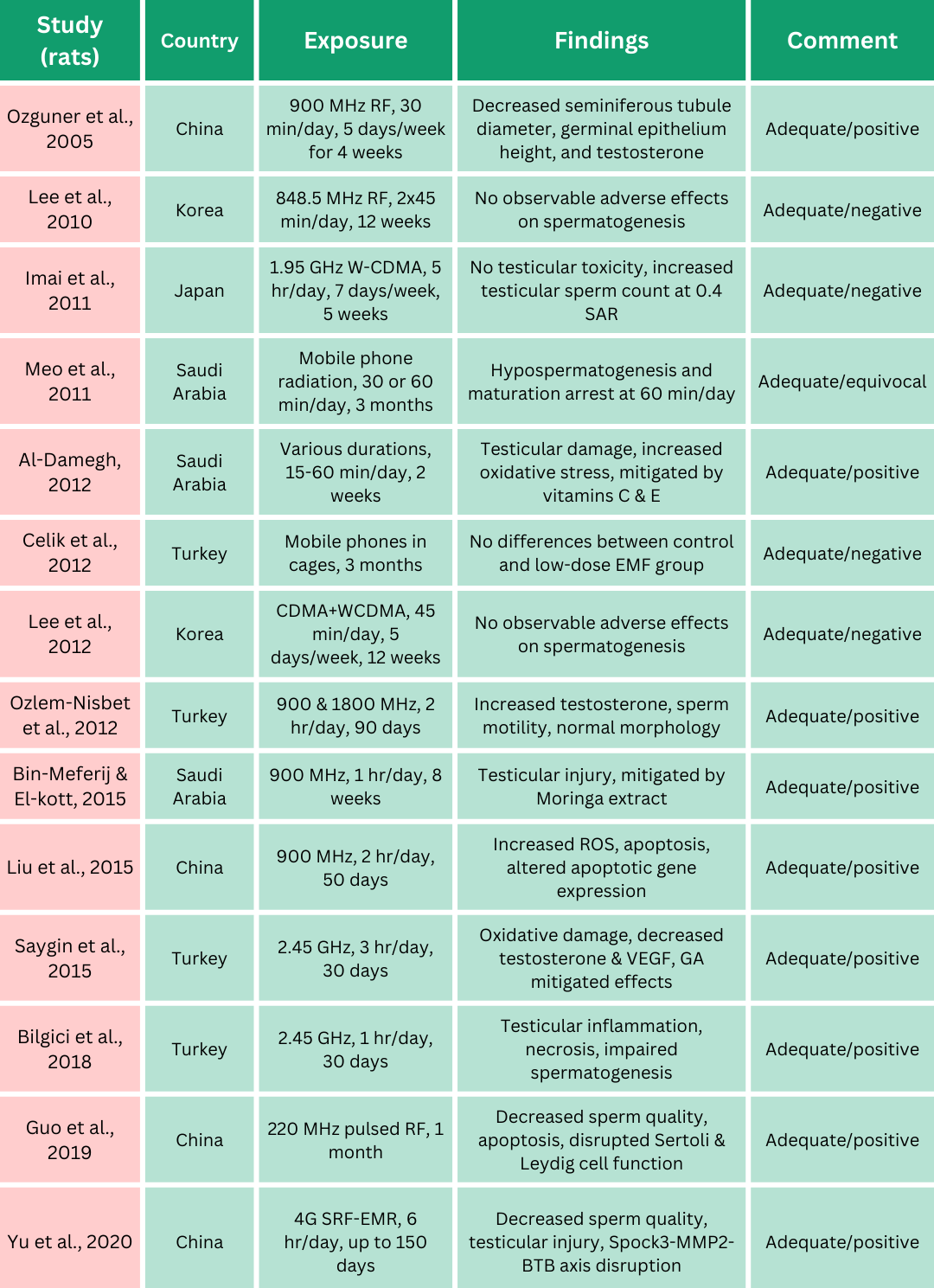
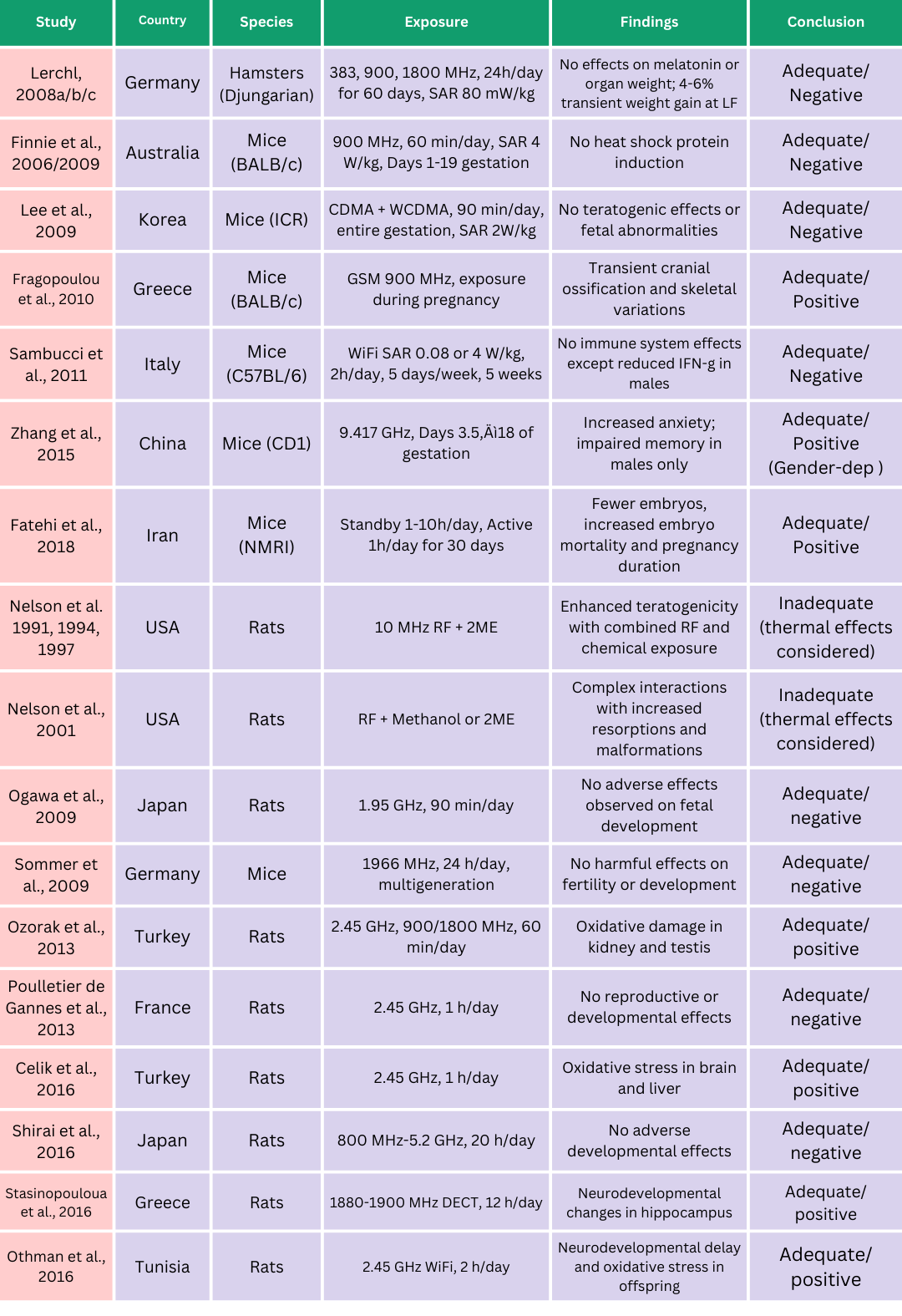
Some In-vitro and animal studies report reduced sperm quality in relation to RF-EMF exposure (Yu et al 2021 and Adams et al 2014). Many of the studies selected by the European Parliamentary Research Service on mice, rats, and hamsters summarized below do show an association as well but are subject to the same limitations as those conducted looking at a relationship with some cancers - and many of them do have mixed results, with other animal studies having not replicating those effects.
Here is a KEY takeaway: Many studies cannot or do not appropriately control for a big confounder either: heat. RF can heat things, particularly smaller animals subject to prolonged exposure in experimental studies.
Without accounting for dose (dosimetry) it is hard to weed out effects that can be attributed to RF and those that could be attributed to heat from prolonged RF exposure. RF-EMF exposure has been shown in past studies to alter how rodents perceive heat or to raise their overall body temperature.
Studies in both rats and humans have shown that high ambient temperatures are associated with a decrease in semen volume during ejaculation, a reduction in sperm concentration and total sperm count, and are negatively correlated with sperm motility (the ability to move effectively) and morphology (normal shape and structure), both critical factors for successful fertilization. A study conducted between 2005 and 2023 in Argentina found that semen from men exposed to heat waves had lower sperm numbers and abnormal morphology. Differences were 4–5 times higher in peak heat wave years (2013, 2023).
One study raised testicular temperatures to 40–42°C with microwave exposure, causing infertility. Mieusset et al. found infertile men had scrotal temperatures just 0.4–0.5°C higher than fertile men (although other studies have found increasing temperatures have no effect), and men with heat-intensive jobs (like welders) are at higher risk for oligozoospermia (low sperm count). Luckily these effects have been reported as reversible.
Meta-analyses have found no clear dose-response pattern between RF-EMF exposure levels and observed effects in rodents. Furthermore, as indicated above, most studies used exposure levels higher than what people typically encounter and above international safety limits. Issues like bias, inconsistent results, and publication bias (positive results are more likely to get published) also reduce the confidence in the findings. So while some studies might show that RF-EMF may affect sperm quality or testicular tissue, the evidence is unclear. Even if there are changes in fertility markers, they may not lead to real impacts on reproductive function.
Animal studies can be helpful in that they are internally valid (you can control for things very well within them so you can tease apart what effects are coming from), but this comes at the cost of external validity (the more you control for, the less you represent real-world characteristics). For the most part, data in humans fails to support evidence of an effect (at least an unequivocal one).
While there is some evidence (albeit weak and inconsistent) of the association between RF-EMF exposure and adverse effects on fertility in men across some cohort or case-control studies, meta-analyses of human studies that have evaluated the impact of RF-EMF on sperm quality (often based on mobile phone usage) show no consistent impact of RF-EMF exposure on sperm quality (Liu et al 2014, Yu et al 2021 and Kim et al 2021). This means that changes in sperm quality after RF-EMF exposure were not significant, even when mobile phone usage increased (again, lack of dose-response steers away from causality). This may indicate that in real-world scenarios RF-EMF exposure from mobile phones is unlikely to have an impact on fertility, and there are other confounders at play. One study even showed improvement in sperm counts in users of 4G/5G relative to 2/3G, which counters a dose-response relationship to RF-EMF, but is consistent with the reduction in the phone’s output power over time.Sperm count naturally fluctuates by the hour, day, and month. So to get an accurate picture of a man's sperm quality, it would need to be tracked over an extended period of time.

In all, the epidemiological studies showing some association with fertility in men are subject to strong confounders (read ahead for even more limitations) and self-reported exposures - most of the effects are observed with occupational exposures. Still, even then, the data is too weak and inconsistent to draw meaningful conclusions.
There is very limited and inconclusive evidence of adverse effects on fertility in women and for adverse effects in pregnant women and their offspring for all developmental endpoints examined, including animal studies.

Data Limitations the Prohibit Strong (or any) Conclusions
Many of the studies examining the potential impact of radiofrequency electromagnetic fields (RF-EMF) on fertility and developmental outcomes rely heavily on self-reported exposure, which introduces significant limitations and potential sources of bias. In these studies, participants were often asked to recall and estimate their daily or historical mobile phone usage, duration of calls, proximity to devices, or exposure to other RF sources such as Wi-Fi or base stations. This method is highly subjective and prone to recall bias, particularly when data are collected retrospectively. Individuals may underreport or overreport their exposure based on personal beliefs, health status, or media influence, which undermines the accuracy of the exposure assessment. This can also skew the participants enrolled in a study, biasing toward those with reported incidences of cancer or fertility-related problems.
A key limitation of most studies (all types, In-vitro, animal and epidemiological) is the lack of precise measurement of RF-EMF exposure. Without clear dosimetry, it’s unclear how much radiation people, animals (and sperm!) were actually exposed to. This makes it difficult to know whether the effects are due to RF-EMF itself or other factors, like heat from the device (specially with older phones that could heat up more). For instance, in some studies where occupational exposure was assessed, RF exposure was categorized based on job titles or expert opinion rather than direct measurements, which introduces classification error. Without precise and objective exposure data—such as personal dosimetry, validated usage logs, or environmental measurements—it's challenging to determine whether any observed associations are truly due to RF-EMF or other unmeasured variables.
Additionally, other confounding variables are quite a common concern in epidemiological studies. Many of the cross-sectional and case-control studies did not adequately account for other lifestyle and environmental factors that could influence fertility or developmental outcomes- often associated with increased mobile phone usage. For instance, factors like age, BMI, smoking, alcohol consumption, stress, sleep patterns, poverty, occupational hazards, exposure to chemicals or heat, and socioeconomic status can all affect reproductive health, yet are often not fully controlled for in the analysis. In studies involving developmental outcomes in children, maternal stress, nutrition, education, and lead exposure are just a few of the many variables that can confound results.
Many studies had small sample sizes or were conducted in specific populations (e.g., military personnel, clinic patients, or volunteers), which limits their generalizability. An often overlooked confounder in these studies is the inclusion criteria tied to access to healthcare and diagnostic services, which can strongly influence study findings. Many participants in fertility and developmental studies are recruited from specialty clinics, such as infertility centers or pediatric developmental services, where individuals are already experiencing health concerns. These populations are not representative of the general public, and their inclusion introduces selection bias. People who seek medical help are more likely to have been diagnosed with a condition—partly because they had access to diagnostic tools and professional evaluation—which may inflate the apparent rates of infertility or developmental disorders in the study sample.
Additionally, socioeconomic disparities play a critical role. Individuals from lower-income backgrounds may have increased exposure to environmental risk factors, including RF-EMFs, due to living closer to cell towers or relying heavily on mobile devices for communication and work. At the same time, they may face limited access to healthcare, leading to underdiagnosis or late detection of fertility or developmental issues. Conversely, people from higher-income groups may be overrepresented in clinical research because they are more likely to seek preventive care and diagnostic services. People from higher-income backgrounds may be more likely to pursue infertility evaluations or developmental assessments for their children, leading to higher rates of diagnosis simply due to better detection, not necessarily an increase in the actual prevalence of these conditions. These disparities can distort the observed associations, as differences in health outcomes may reflect inequities in healthcare access and living conditions rather than effects of RF exposure alone.
In data sets tracking incident rates over time, the improved detection rates for specific types of cancer (from better imaging and diagnostic criteria) may confound the analyses, lending credence to the idea that cancer rates are increasing with increased phone usage when in reality they are just increasing due to better diagnostic criteria and imaging.
In short, when inclusion in a study depends on diagnosed conditions and diagnostic access is influenced by poverty and systemic inequities, these become powerful confounding factors. Without accounting for such socioeconomic and healthcare disparities, the validity of observed associations between RF-EMF exposure and health outcomes remains uncertain- which explains the inconclusive and mixed nature of the data available.
Altogether, these methodological limitations highlight the need for more robust, well-designed studies with objective exposure assessments and better control of confounding variables to clarify the relationship between RF-EMF exposure and reproductive or developmental effects. Lastly, it is quite important to highlight that a review of the data suggests that the potential decline in male sperm counts does not necessarily translate to a decline in male fertility.
About this team:
David Robert Grimes is a mathematical modeller, medical researcher, broadcaster, and author. He is an expert in the public understanding of medical science, and contributes to outlets including the Guardian, Scientific American, The New York Times, The BBC, the Financial times. Irish Times, and more. He appears frequently in the news media on topics and his research focuses on public understanding of science, research integrity, and mathematical modelling. He was joint recipient of the 2014 Nature/Sense about Science John Maddox Prize for standing up for science and is a fellow of the Committee for Skeptical Inquiry. He is the author of "Good Thinking - Why flawed logic puts us all at risk and how critical thinking can save the world" (The Experiment, 2021).
Nini is a proud Colombian from Barranquilla with a multidisciplinary background that spans sensor design, neural interfaces, and a strong emphasis on nanofabrication, data science and statistics, process control, and risk analysis. Beyond her technical expertise, she’s also a wife and mom to a spirited little girl. TECHing it Apart was born from Nini’s passion for sharing deep, accessible insights on the topics she covers on Instagram @niniandthebrain. There, she breaks down misinformation that distorts public health policy and misleads consumers—often through flawed methodology or data manipulation—as well as explores trends in health technology.
All content is freely available, but as an independent writer and researcher, Nini appreciates support from those who value this work.