Unregulated, Unproven, Unaccountable: How Lack of Oversight in Wellness Led to a Child’s Death
The hidden cost of wellness: When emotional, anti-science anecdotes outweigh scientific consensus, the results can be deadly—costing lives, resources, and the chance for real solutions.
A worst-case scenario has played out in the wellness world: a child has died. In this tragic case, a 5-year-old boy died while receiving treatment in a hyperbaric chamber operated by an integrative medicine provider (it is unclear what for, but it is rumored from the Nursing Subreddit it was for ASD, which makes this even more tragic and problematic), the Oxford Center, in Troy, MI. It is key to highlight that, according the latest information provided, the Oxford Center is not a licensed or accredited medical facility for hyperbaric oxygen nor is it a hospital subject to rigorous healthcare standards. The Michigan Department of Licensing and Regulatory Affairs (LARA) said that state law does not require hyperbaric oxygen facilities to be licensed or regulated by LARA. This distinction is crucial because alternative medicine clinics often lack the safety protocols, emergency medical response, and trained personnel found in hospitals.
A hyperbaric chamber is a pressurized medical device designed to deliver 100% oxygen at higher-than-normal atmospheric pressure. It is most commonly used in hospitals to treat decompression sickness (the "bends"), carbon monoxide poisoning, severe infections, and non-healing wounds. In medical settings, hyperbaric oxygen therapy (HBOT) is conducted under strict clinical supervision with trained professionals ensuring safety protocols are followed. The FDA clearly states that because of the risk of fire, one should only use hyperbaric chambers in accredited facilities by the Undersea and Hyperbaric Medical Society, though accreditation is not a requirement. The UHMS map shows that only two accredited hyperbaric facilities exist in Michigan, located in Grand Rapids and Niles—the Oxford Center is not among them.
Hyperbaric chambers have become popular in alternative and integrative medicine, where they are often used to treat conditions not approved by the FDA, such as autism, Lyme disease, and chronic fatigue syndrome. Unlike hospital-based hyperbaric treatments, integrative medicine providers may operate these chambers without the same level of medical oversight, regulatory compliance, or emergency preparedness.
The Oxford Center claims to treat a laundry list of unrelated conditions, including glaucoma, interstitial cystitis, cancer (without specifying which type), hearing loss, heart conditions, infections, diabetes, depression, dementia, traumatic brain injury (TBI), rheumatic diseases, and even sickle-cell disease—essentially positioning itself as a one-stop shop for curing nearly everything.
This is a classic red flag of wellness, marketing alternative treatments as universal cure. Legitimate medicine operates within scientific constraints, acknowledging that different diseases require specialized treatments based on extensive clinical research. In contrast, wellness sidesteps scientific validation by promoting unproven therapies as miracle solutions for a vast range of conditions, often prioritizing anecdotal "data" over rigorous, peer-reviewed one.
By offering a one-size-fits-all approach, they appeal to a wide range of vulnerable people looking for answers, especially those with complex, poorly understood, or difficult-to-treat conditions. The fact that the Oxford Center markets itself as treating such a vast and unrelated range of conditions—many of which require highly specialized care—suggests that their primary goal is financial gain rather than genuine medical advancement. This is not just misleading—it is dangerous.
The choice that never was
When it comes to wellness, people often focus on the potential gains—improved health, increased energy, or enhanced well-being—while rarely considering the costs associated with those choices. This is where the concept of opportunity cost comes in, a key concept applicable to all aspects of life.
Opportunity costs refer to the benefits missed when one choice is made over another. Think about it as an investment you don’t make because you choose another investment (buying a house vs. investing into stocks, for instance). In the context of wellness, this means that every choice—whether it’s investing in an alternative treatment, following a strict diet, or dedicating time to a specific regimen—comes at the expense of something else.
For example, choosing an expensive wellness treatment like IV therapy or hyperbaric oxygen sessions might mean less money for proven medical care, nutritious food, or other essential needs, or in the worst case, higher risks of fatal outcomes.
Failing to consider opportunity costs can lead people to invest time, money, and effort into ineffective wellness trends while overlooking evidence-based health solutions that could provide greater benefits in the long run.
The Hidden Cost of Alternative Medicine: Understanding opportunity costs under the illusion of safety
When conventional medicine fails to provide clear answers, the allure of alternative therapies becomes undeniable. These approaches often present themselves as natural, holistic, and free from the bureaucracy and perceived coldness of modern healthcare. Anecdotes of miraculous recoveries, testimonials of life-changing results, and the certainty with which these therapies are marketed help quell the epistemic uncertainty we struggle to accept about our own health. At first glance, the harm in choosing these interventions might seem minimal—they appear harmless, sometimes even gentle, and promise hope where traditional methods fall short.
However, in healthcare, this means that every decision to pursue an unproven treatment comes at the expense of potentially more effective, evidence-based options. This cost isn't just financial—it involves delayed interventions, worsening health outcomes, emotional distress, and systemic consequences that ripple through public health initiatives.
The Loss of Evidence-Based Health Improvements
Modern medicine is not without flaws, but it is built upon a foundation of scientific rigor. Treatments are supported by extensive research, clinical trials, and evidence demonstrating their safety and efficacy. Choosing alternative therapies over proven interventions can mean missing critical windows of opportunity for treatment, especially in conditions where timing is everything—such as aggressive cancers, heart disease, or progressive neurological disorders.
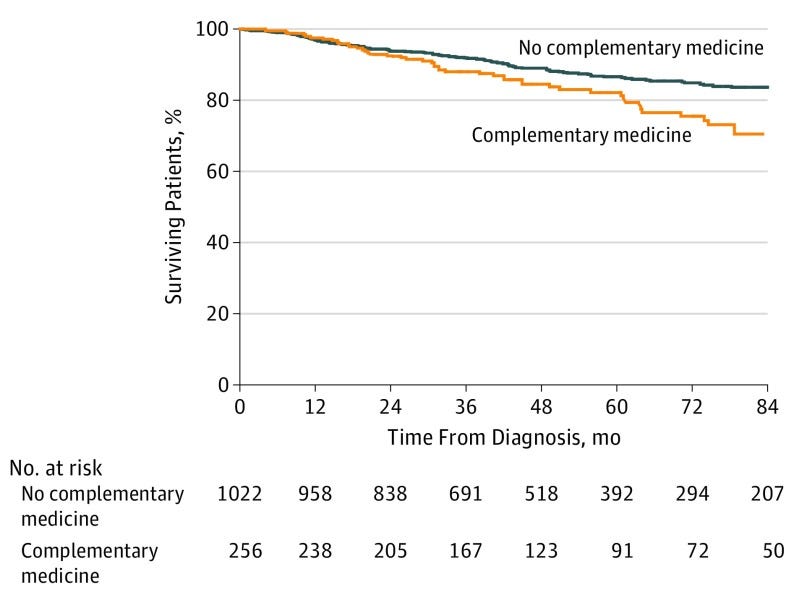
For instance, studies have shown that cancer patients who rejected conventional treatments in favor of complementary or alternative therapies faced twice the risk of death compared to those who followed evidence-based physician recommendations. This increased risk was primarily due to delays in or complete refusal of scientifically validated treatments. When an unproven treatment fails, the consequences are not just an unchanged status quo—they are often worsened conditions that could have been managed or even cured if addressed earlier.
The Financial Burden of Ineffective Treatments
Healthcare is expensive. Whether it’s out-of-pocket costs for individuals or larger systemic costs borne by public health systems, every dollar counts. Alternative therapies are often marketed with the promise of affordability and accessibility, but the reality is far less forgiving. Many of these interventions require repeated sessions, costly supplements, and ongoing consultations that can quickly add up. Worse still, when these treatments fail—or cause harm—patients often return to conventional medicine with more severe conditions, leading to longer hospital stays, additional procedures, and higher expenses.
The financial toll isn’t limited to individuals. Healthcare systems also suffer when resources are redirected to address complications stemming from unregulated treatments. Funds that could have been allocated to research, public health programs, or preventive care are instead absorbed by the fallout of ineffective interventions.
The Emotional and Psychological Toll
Health isn’t just physical—it’s deeply emotional and psychological. Patients who invest in alternative therapies often do so with significant emotional commitment. The hope, faith, and belief they place in these treatments carry immense psychological weight. When these interventions fail, the emotional fallout can be profound: feelings of guilt, regret, and self-blame are common, especially when patients are told that their lack of improvement is due to not believing strongly enough or not following the protocol “perfectly.”
Additionally, trust in medical professionals is often eroded. After experiencing failure with alternative treatments, some patients become skeptical of all healthcare providers, delaying further care or refusing evidence-based interventions altogether. This erosion of trust can have lasting consequences, perpetuating cycles of misinformation and poor health outcomes.
The Broader Societal Impact
The effects of choosing alternative medicine over evidence-based care extend beyond individual health outcomes—they impact society at large. As pseudoscientific treatments gain popularity, public health initiatives often suffer. Resources that could be directed toward disease prevention, vaccination campaigns, or public education are instead diverted to counter misinformation and repair damage caused by ineffective treatments.
Moreover, the normalization of pseudoscience undermines trust in healthcare institutions and scientific research. Misinformation spreads quickly, fueled by survivor stories and anecdotal evidence that dominate headlines, while stories of treatment failures or preventable deaths remain hidden. This imbalance skews public perception, making it even harder to advocate for evidence-based solutions.
Hidden Dangers Behind the Illusion of Harmlessness
Not all alternative treatments are harmless. While some may indeed pose little direct physical risk, others can be actively dangerous. Without proper oversight and regulation, issues of dosage inconsistencies, contamination, and unverified safety claims become serious concerns. Natural does not always mean safe, and the absence of side effects does not mean the treatment is effective.
Furthermore, the wellness industry often operates in a space with minimal accountability. If a patient suffers harm from an unregulated supplement or therapy, there is little legal recourse. This lack of oversight creates an environment where claims can be exaggerated, failures can be hidden, and blame can be redirected onto patients themselves.
The Survivor Bias Problem
One of the most powerful tools in the wellness industry’s arsenal is the survivor story. These anecdotes are emotionally compelling, easy to share, and hard to dispute. Yet, they suffer from survivorship bias—we hear only from those who claim to have benefited, while those who did not improve or even worsened remain invisible.
When someone using alternative therapies for cancer later dies from the disease, their story rarely makes headlines. Meanwhile, a single story of someone who credits their survival to a questionable remedy spreads like wildfire. This selective storytelling creates a distorted narrative, reinforcing the illusion of effectiveness while hiding the far more common reality of failure.
I will separately discuss other statistical effects that given the illusion that wellness works - even though it likely does not. I have summarized some of these here:
But Isn’t Modern Medicine Flawed Too?
It’s essential to acknowledge the imperfections in conventional healthcare:
Administrative inefficiencies and bureaucratic delays are common.
Costs remain extraordinarily high in many countries.
Racial and gender disparities persist in access and outcomes.
Clinical trials often lack diversity and inclusivity.
Yet, despite these flaws, evidence-based medicine remains our best option. It is transparent, accountable, and—most importantly—self-correcting. When errors are discovered, protocols are revised. When harm is detected, treatments are withdrawn and health policy is changed accordingly. Science evolves, adapts, and strives for improvement.
Wellness loves to pit evidence-based medicine against common-sense lifestyle modifications—such as better sleep, lower stress levels, exercise, and a balanced diet—but, as I have discussed before, this is a false dichotomy. In reality, these approaches are not mutually exclusive; true healthcare integrates both, recognizing that while lifestyle choices play a crucial role in well-being, they cannot replace medical interventions for serious conditions.
Ironically, many folks who vehemently defend this space claim every interaction matters (when recommending supplements or other unproven interventions) while almost blatantly ignoring the effect (and interaction) of confounders that likely contribute the most to improvement (diet, exercise, better sleep, and stress reductions...and well, time).
They will say things like: “Every person is different!'“ or “What works for one may not work for another.” This argument conveniently ignores that medicine works despite these individual differences. If a treatment only “works” for a few people but not when tested scientifically, then it probably doesn’t work at all. The irony is that medicine already accounts for these differences, as treatments are tested across diverse groups, side effects are tracked/reported and statistical testing helps separate real effects from random chance.
In contrast, the wellness space often refuses to acknowledge its shortcomings. It rarely admits fault, rejects criticism, and instead shifts blame onto patients for their supposed lack of belief or discipline.
Conclusion: Choose Evidence Over Illusion
The harm of alternative medicine isn’t always in what it does (or doesn’t do)—it’s in the missed choices. The lost opportunities, delayed treatments, wasted financial resources, emotional distress, and societal consequences form a heavy toll that is often invisible until it’s too late.
When it comes to health, hope isn’t enough. Anecdotes aren’t data, and survivor stories aren’t proof. True care requires evidence, accountability, and an unwavering commitment to outcomes that can be measured, replicated, and trusted.
Science isn’t perfect, but it’s the best tool we have. And when lives are on the line, it’s the tool we must choose—every single time.
I'm Nini, a proud Colombian hailing from Barranquilla. My expertise spans from sensor design to neural interfaces, with emphasis on nanofabrication, data science & statistics, process control, and risk analysis. I am also a wife and a mom to one little girl. TECHing it Apart emerged from my drive to share in-depth insights on topics I cover on Instagram (@niniandthebrain), where I dissect misinformation that skews public health policy and misleads consumers through poor methodology and data manipulation, as well as trends in health technology. Content here is free, but as an independent writer I sure could use your support!









The term "Wellness" has been hijacked by the charlatans who peddle all sorts of misinformation and mistreatments for profit. "Wellness" used in marketing should be a red flag for everyone. Thanks for your great work Nini.